Partners provides DEXA services:
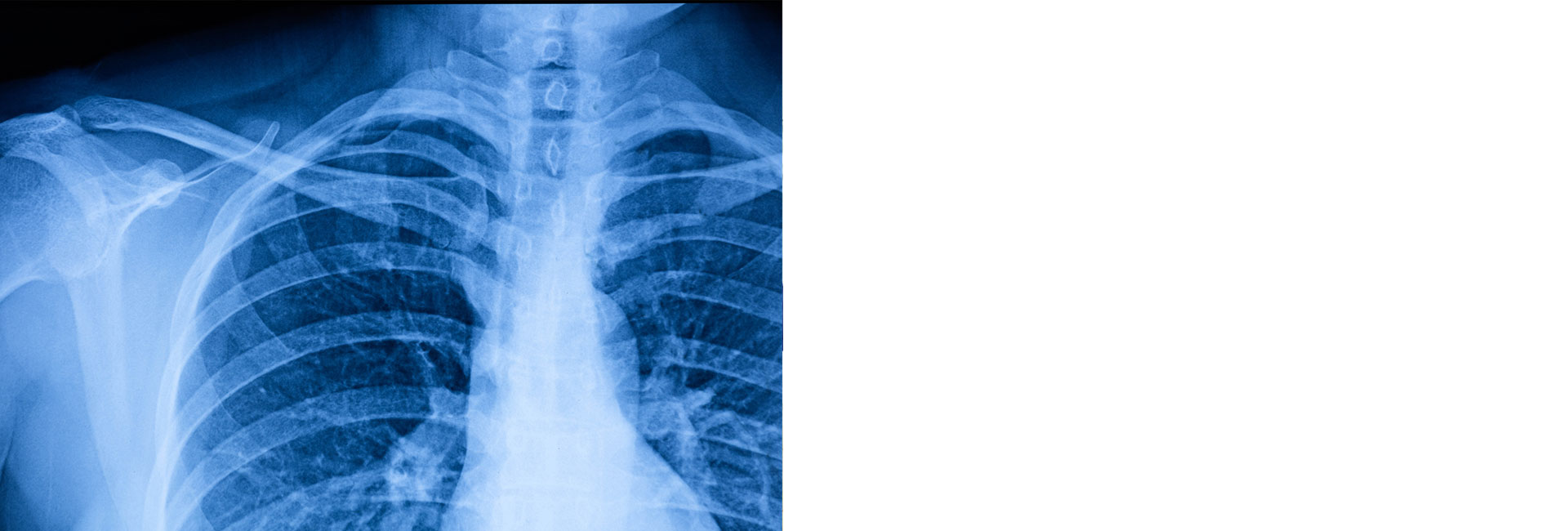
Dual Energy X-ray Absorptiometry (also known as: Bone Mineral Densitometry)
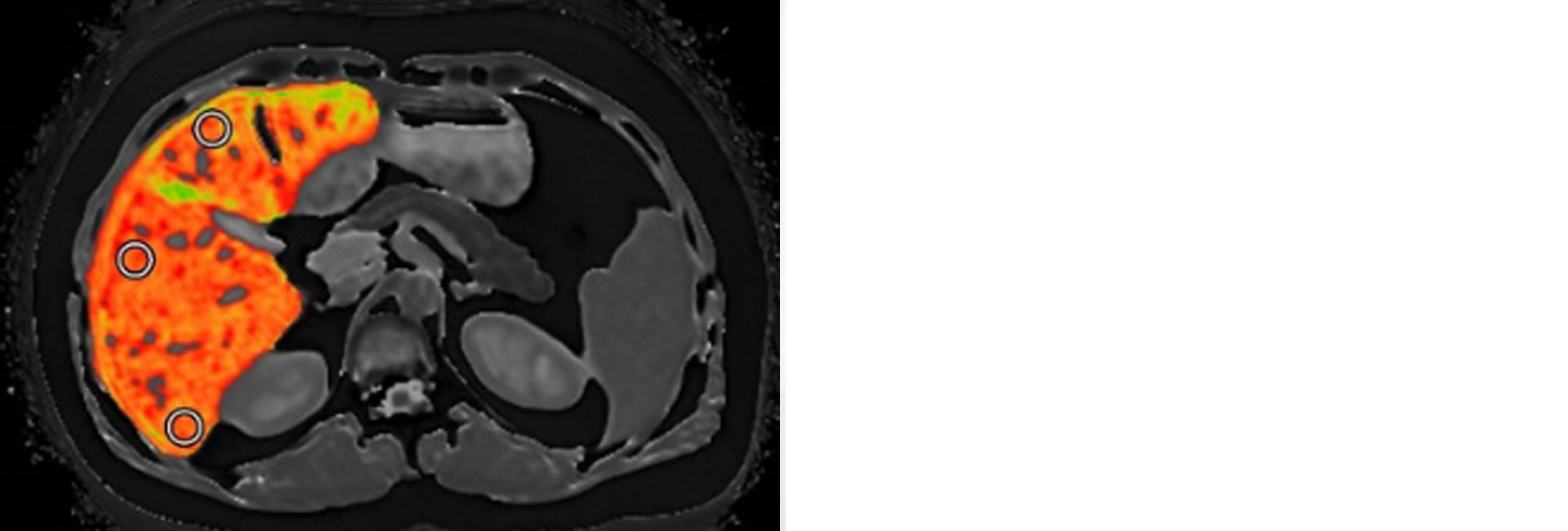
Body Composition Analysis :
The Body composition measurement using a DEXA scan is a simple seven minute scan that provides a comprehensive look at your body fat, lean mass and bone density with scientifically validated accuracy. Beyond body composition, a DXA scan will provide you with insights in to health risks like visceral adipose tissue, bone density, estimates of skeletal muscle mass. A detailed, comprehensive report will help you identify health risks and more accurately track changes in body composition over time.
Click HERE for more details.
Osteoporosis:
Osteoporosis is a silent, progressive disease characterized by decreased bone density and increased bone fragility, with a consequent susceptibility to fracture.
 In the United States, over 28 million people are at high risk of developing osteoporosis. Up to 1.5 million fractures a year are attributable to osteoporosis. Women are at the greatest risk. One third of Caucasian women over the age of 50 have osteoporosis, yet nearly 80% remain undiagnosed. After menopause, a woman’s risk of suffering an osteoporotic spine or femur fracture is 30% or three times that of a man’s.
In the United States, over 28 million people are at high risk of developing osteoporosis. Up to 1.5 million fractures a year are attributable to osteoporosis. Women are at the greatest risk. One third of Caucasian women over the age of 50 have osteoporosis, yet nearly 80% remain undiagnosed. After menopause, a woman’s risk of suffering an osteoporotic spine or femur fracture is 30% or three times that of a man’s.
Osteoporosis is a complex, multi-factorial disease that may progress silently for decades; there may be no symptoms until fractures occur. Bone loss is the major risk factor that can be modified in mid-life to reduce fracture risk. Bone loss can be reduced by treatment, but it is difficult to restore the microarchitecture of the skeleton once bone has been lost. Early detection and intervention are crucial.
The Role of Densitometry
Bone densitometry is an essential tool in osteoporosis management. Densitometry assists physicians in diagnosis, fracture risk assessment, and monitoring response to therapy.
Diagnosis of Osteoporosis
Physicians utilize bone densitometry to categorize patients as normal, osteopenic, or osteoporotic following the World Health Organization (WHO) classifications. The patient’s T-score (comparison to the young adult reference) is the critical variable in diagnosis. Typically, both femurs and the spine are assessed, with the diagnosis made using the lowest T-score. Patient examination, in addition to the T-score, is key to diagnosing osteoporosis.
Fracture Risk Assessment
Bone mineral density (BMD) is the strongest tool to predict fracture risk, which increases exponentially as BMD decreases. Femur BMD is recognized as the strongest predictor of femur fracture risk, which has the highest morbidity, mortality and cost of all osteoporotic fractures. A decrease of 1 standard deviation (SD) in femur BMD corresponds to approximately a 3X increase in femur fracture risk. In comparison, a 1 SD decrease in spine BMD corresponds to a 2X increase in spine fracture risk.
The AP Spine is an ideal site for measuring a patient’s bone mineral density. This is due to the fact that it is a weight bearing area and is prone to osteoporotic fractures. The spine’s high concentration of metabolically active trabecular (soft, spongy) bone makes it the most sensitive site for monitoring response to therapy.
Monitoring Changes in BMD
Patients may return for bone density tests every 1-3 years, depending on the expected rate of loss and their clinical situation. BMD may increase over time as a response to therapy, or it may decrease with disease progression or poor response to therapy. Precision (reproducibility) of the BMD measurements is the key factor in detecting changes in patient BMD over time.
Our GE Lunar bone densitometers continue to set new landmarks in clinical value with high-performance applications, advanced clinical utility, and the unique enCORE™ software platform